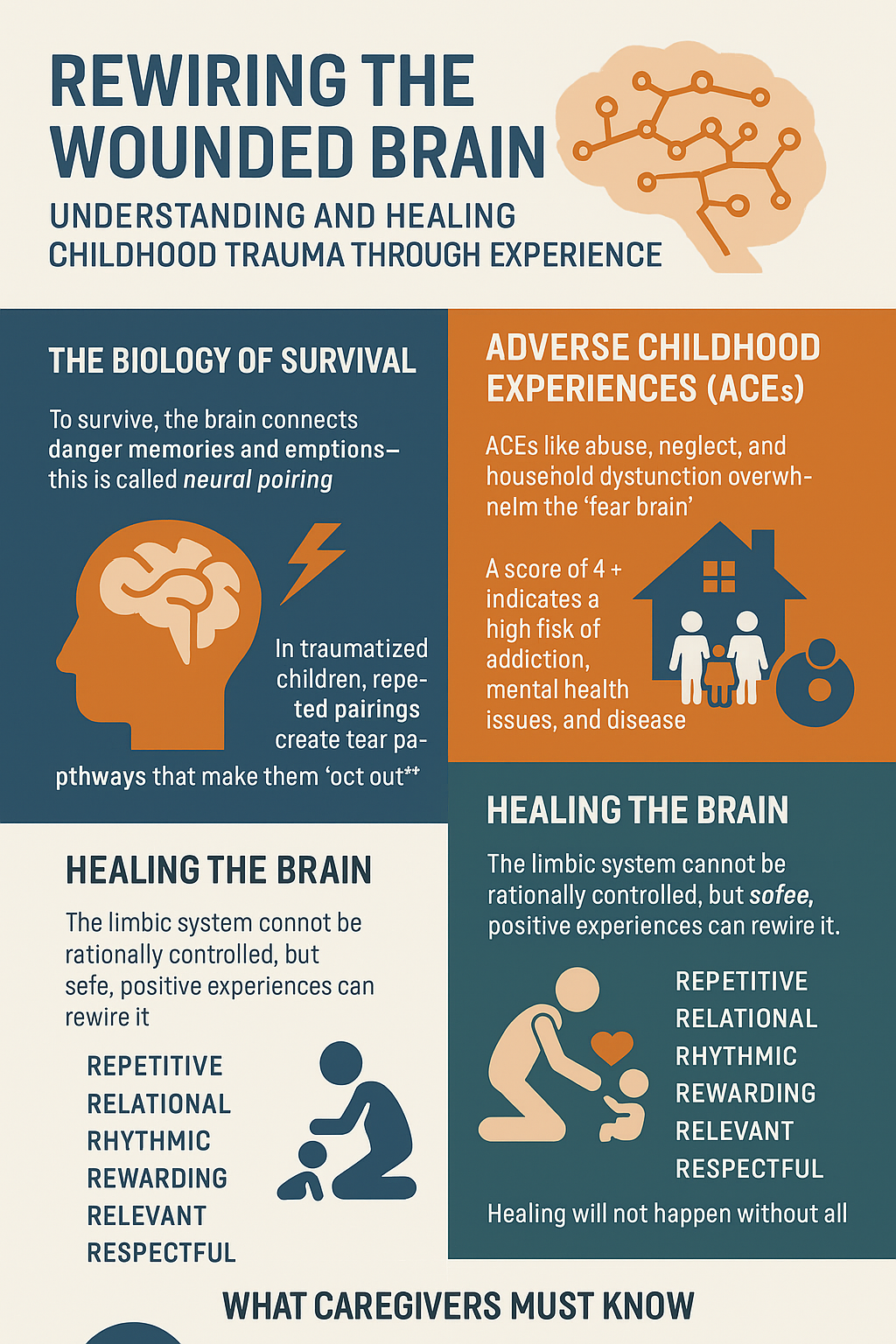
When working with traumatized youth, one must look beyond behavior and see the brain behind it. Traumatized teens aren’t just troubled; their neurobiology has been rewired by repeated experiences of fear, neglect, and abuse. To support their healing, we must first understand how the brain adapts to trauma—and how it can adapt again through safety, consistency, and relational care.
I. The Biology of Survival: How Trauma Rewires the Brain
The human brain is built for survival. Through a process known as neural pairing, experiences that occur repeatedly or intensely get “wired together.” For instance, a child who hears a garage door may not react—unless they grew up associating that sound with danger, such as an abusive parent returning home. That sound then becomes a trigger, instantly activating the body’s fear response before conscious thought even begins.
This is an adaptive function. It’s what allows us to run from a threat without debating it. But for traumatized children, what fires together wires together in dangerous ways:
- Touch becomes associated with abuse.
- Authority becomes linked with betrayal or danger.
- Home becomes a site of fear, not safety.
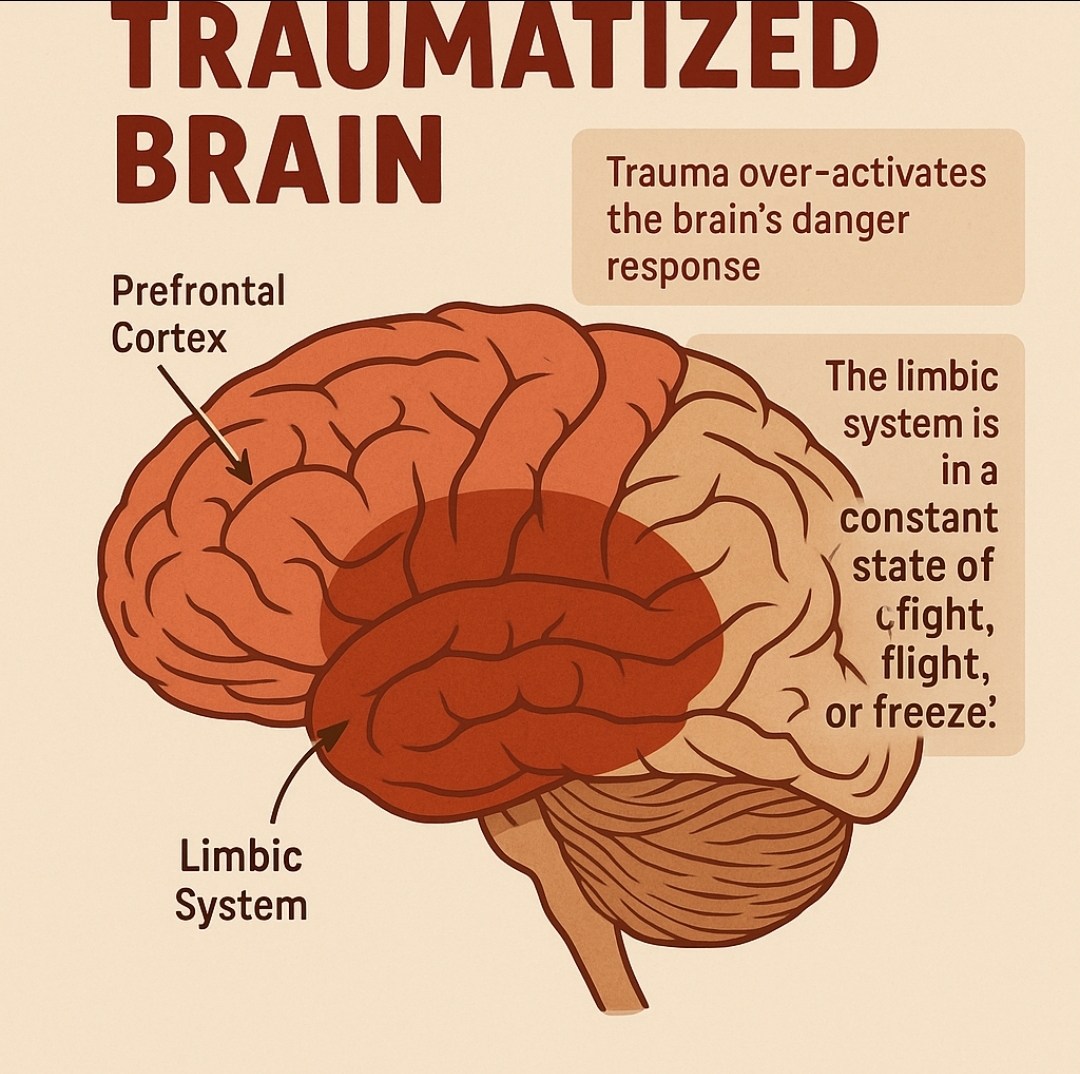
These associations get stored in the limbic system, the brain’s emotional center. It’s this part of the brain—responsible for fight, flight, or freeze—that dominates in traumatized youth. Functional MRI scans show that trauma-affected brains have an overactive limbic system and an underactive prefrontal cortex (the thinking, reasoning part of the brain). This means that when a teen “flips out,” they’re not misbehaving—they’re surviving.
II. The Triune Brain and “Flipping the Lid”
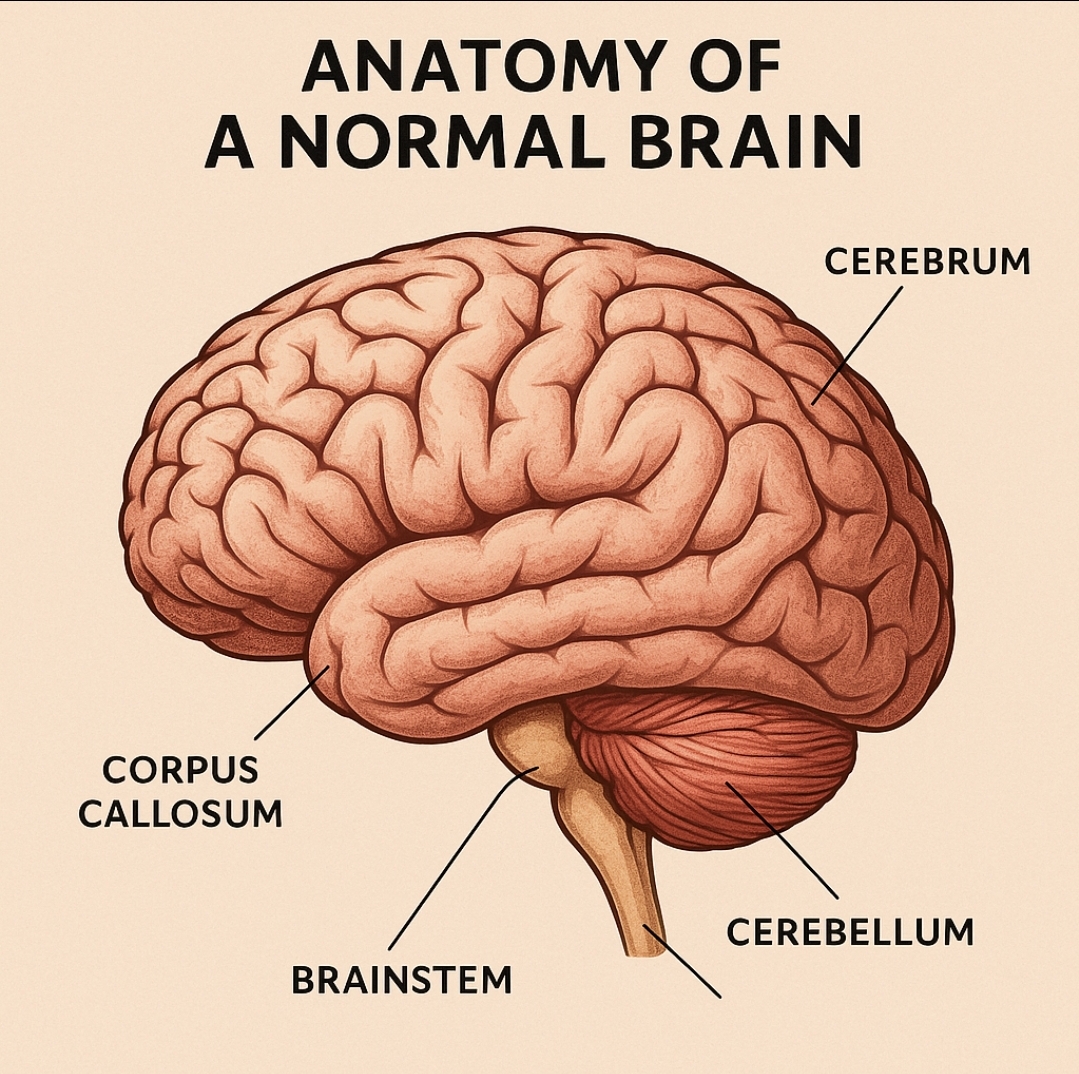
Dr. Dan Siegel’s model of the triune brain breaks the brain into three parts:
- Brainstem – Controls basic life functions (breathing, heart rate).
- Limbic System – Processes emotions and fear; initiates fight/flight/freeze.
- Prefrontal Cortex – Enables reasoning, reflection, language, and morality.
In trauma-affected children, the prefrontal cortex often goes offline, leaving only emotional reflexes and survival behaviors. This explains why traditional discipline or rational explanations fail: you’re talking to the wrong part of the brain.
III. Adverse Childhood Experiences (ACEs): A Root of Lifelong Consequences
The landmark ACE Study by Drs. Vincent Felitti and Robert Anda revealed ten types of childhood trauma that strongly correlate with later-life struggles:
- Abuse (physical, emotional, sexual)
- Neglect (physical, emotional)
- Household Dysfunction (domestic violence, substance abuse, mental illness, incarceration, divorce)
A score of 4 or more ACEs drastically increases the likelihood of addiction, depression, poor academic performance, obesity, heart disease, and even early death.
Why? Because the toxic stress from these experiences keeps the limbic system constantly activated, flooding the body with cortisol and adrenaline. This hormonal bath gradually degrades physical and mental health, rewiring behaviors to focus solely on survival.
IV. Healing the Brain: Experiential Repair Through Safe Relationships
Here’s the hope: if trauma is experientially created, it must be experientially healed. Neural pairings cannot be undone—but they can be overridden by stronger, safer connections. This is where relational caregiving becomes sacred.
Healing is grounded in the 6 R’s from Dr. Bruce Perry:
- Repetitive
- Relational
- Rhythmic
- Rewarding
- Relevant
- Respectful
These six principles guide every intervention, whether it’s caring touch, animal-assisted therapy, experiential adventures, or simple moments of attuned listening. Every safe, positive interaction is a seed of rewiring.
For example, if a child fears physical touch due to sexual abuse, a consistent pattern of safe, nurturing, and non-threatening contact—perhaps petting a dog or receiving a comforting high-five—can build a new neural path that redefines touch as safety.
V. What Trauma-Informed Caregivers Must Know
- Behavior is communication. A meltdown is often a fear response.
- Don’t take it personally. Teens lash out from a place of survival, not malice.
- Words don’t heal trauma—experiences do. Rational talk only helps when the limbic system is calm.
- Consistency rewires. The brain needs repeated safety to trust.
- Love requires boundaries. Safe, respectful limits communicate worth.
Caregivers aren’t just staff—they are healing agents in a child’s internal war zone. Every safe experience offered is a vote against the pain of the past.
Conclusion: From Surviving to Thriving
To heal a traumatized teen is not to lecture them—it is to retrain the brain through the power of experience. Trauma made their world dangerous; you must make it safe. The limbic brain needs proof—not words—that people can be trusted, that emotions can be safe, and that life can be worth living.
It’s a battlefield for the soul, where fear is slowly replaced with connection, chaos with rhythm, and despair with hope. Through the work of trauma-informed care, a future is not just possible—it’s being built neuron by neuron, heart by heart.